Ultrasound Measurements
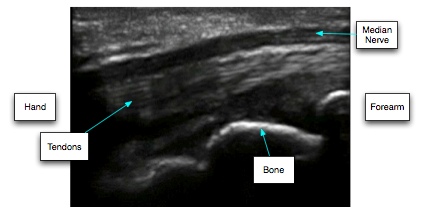
The carpal tunnel is a complicated 3-dimensional structure with a variety of different tissues within and around it. The scanners in routine use for this show you 2-dimensional 'slices' through this structure, the orientation depending on how you hold the ultrasound transducer. The first thing one appreciates when starting to look at it with an ultrasound scanner is that it is generally very easy to see the median nerve itself. In longitudinal sections, when the plane of the scan is aligned along the course of the nerve it generally appears as a dark (hypo-echoic) structure with a bright (hyper-echoic) line above and below it which is generated by the tough fibrous 'sheath' which surrounds the entire bundle of cells which constitute the nerve. Often this bright line is better seen at the side of the nerve nearer to the transducer.
Turn the ultrasound transducer through 90 degrees so that the plane of the scan is across the wrist and perpendicular to the course of the nerve and you then see the nerve as an irregularly shaped round/oval/triangular structure. Again the centre of the nerve is dark (hypoechoic) and the nerve sheath appears as a bright line surrounding it. It is often possible to see the entire circumference of sheath around the nerve but not always.
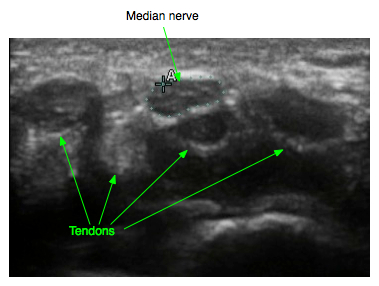
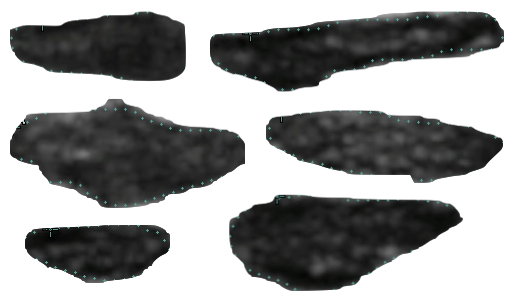
The nerve can be distinguished from the surrounding tendons by the way the tendons move with finger movement and by the fact that the tendons change markedly from dark to light in the ultrasound image with slight tilting of the transducer - a property known as anisotropy. The shape of the nerve in transverse section varies widely from individual to individual:-
It was already known from CT and MRI imaging studies that the median nerve showed enlargement in CTS so the obvious first thing to try and measure with an ultrasound scanner was the size of the nerve, and this is where even the simplest approach to ultrasound of the carpal tunnel starts to get more complicated. If one thinks of the nerve in the simplest way possible as a cylindrical structure then how do you measure the size of a cylinder? We can measure it's diameter in a lengthwise section, but if it is not round but a more irregular shape it will have several different diameters depending on the direction in which we make the measurement and even a round cylinder is subject to measurement errors if we do not measure across the widest part but are slightly 'off centre'. Most ultrasonographers have concluded that it is easier to make reliable measurements by looking at the cross-section of the cylinder. Again one has to be careful about the orientation of the transducer. If the scan plane intersects the tubular structure of the nerve at an oblique angle, either from side to side or in the superficial to deep directions then this will affect measurements of the cross-section. These images are of the same nerve, at the same point (where the true transverse cross sectional area is 9 mm sq)
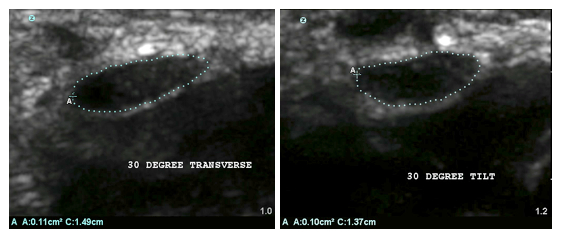
It is however generally easier to maintain the required right angle to the line of the nerve in transverse views than in longitudinal ones. This reliance on transverse views however introduces another complication. If the nerve was a uniform cylinder then a transverse section anywhere along it's length would be the same. However the median nerve is not a uniform cylinder, especially not in carpal tunnel syndrome. It changes in both shape and size as you move along the nerve from the forearm to the hand. One is therefore faced with a choice of levels at which one can pick a transverse section to measure. Most studies have chosen to standardise their 'level' (or levels - one can make more than one measurement of course) by reference to anatomical landmarks such as the pisiform bone or the hook of the hamate bone, or the distal wrist crease (which closely approximates to the pisiform bone). This is easy to teach to a new ultrasonographer but is confounded by the fact that the median nerve is not actually longitudinally fixed in place in relation to these landmarks. With movement of the wrist and fingers the normal median nerve slides up and down through the carpal tunnel and a transverse scan taken at the wrist crease can change in appearance as the wrist and fingers move and a different bit of nerve slides into view or as the tendons push the nerve around and deform its outline.These two images were captured by keeping the transducer stationary at the distal wrist crease and simply opening and closing the fingers:

Some authors have therefore adopted the strategy of simply measuring the biggest bit of nerve they can identify in the region of the carpal tunnel and just proximal to it.
Even once we have decided to make transverse measurements and chosen a level or levels at which to make them we are still faced with a choice of methods for evaluating the size of an irregularly ovoid object.This is an unmarked transverse scan of my left median nerve recorded using the highest frequency setting of the transducer and magnified as much as the machine permits.

Some early studies were limited by the measurement capabilities of their scanners, some of which only provided the facility to measure the linear distance between two points on the scan. There are thus studies in which the nerve size is measured as the transverse diameter, as judged by the operator. Possible measures that could be made on this image include:
A little more sophistication appeared when people began to measure both the largest and smallest diameters on one of these images. If one accepts the approximation that the nerve can be considered to be an ideal ellipse then its cross-sectional area can be calculated from these two diameters. Applying the formulae for the area of a ellipse to the above images yields area estimates of 9.4 sqmm or 10.4 sqmm depending on which short axis measurement is chosen. Scanner manufacturers also allow you to draw a perfect ellipse on the image and adjust it to try and obtain the best fit:

Most recently scanners have provided the facility to trace around the outline of an irregular structure and the machine will then calculate the area enclosed within the outline, as seen in the first transverse image above, and this seems to be the best approach to measuring one level of median nerve transverse section but even here there is scope for differences in practice when it comes to tracing the nerve outline - should one draw around inside the nerve sheath, directly along the bright hyperechoic nerve sheath, or right round the outside trying to include the entire nerve structure. The most reproducible of these choices when used by different operators appears to be to draw the boundary 'just inside' the nerve sheath and this is the practice in Canterbury. The image we have been looking at here gives a cross sectional area of 9 sq mm when measured like this. In this case the fitted ellipse and the outline tracing method give the same answer but the more the nerve shape departs from an ellipse the more these methods will disagree.
Some nerves present you with additional problems. Although in most subjects the median nerve at the carpal tunnel is a single structure, in some patients it starts to divide into branches above the carpal tunnel and a transverse image may show two:-
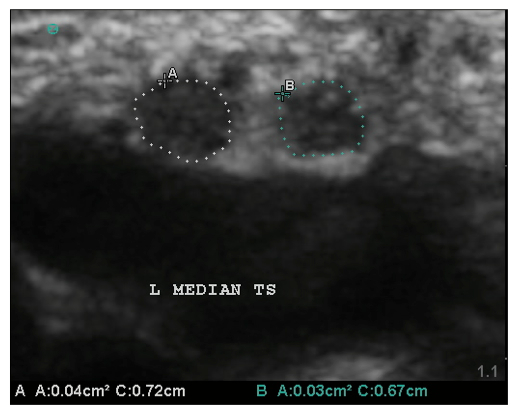
... or even three nerves, providing yet more choices in how to measure them - measure them all individually and add them together, draw a boundary which goes round them all (which may be what the nerve sheath does in some cases), or just conclude that these cannot be measured and compared with subjects who only have a single nerve trunk at the carpal tunnel.
It has taken three rather lengthy paragraphs to explain in detail the complexities of making a single measurement of a cross-sectional area of a median nerve. There are however many further possibilities:
Multiple Measures - We can make as many cross sectional measurements as we wish, in the forearm, carpal tunnel and hand and combine them into derived measures by adding them, subtracting them, or calculating ratios of one measurement to another.
Bowing of the transverse carpal ligament - moving away from the median nerve we can look at the shape or size of the carpal tunnel itself, or especially at the extent to which the transverse carpal ligament bulges outside a straight line drawn between its bony attachments at either end.
Nerve mobility - as mentioned above the normal median nerve slides up and down through the tunnel with wrist and finger movement and also moves in a transverse plane in relation to the flexor tendons. Both of these movements may become restricted in CTS and attempts have been made to measure them
Nerve texture - although the normal median nerve at the wrist is a fairly hypo-echoic structure on ultrasound, following it a little way up the arm will show that more proximally there is usually much more internal structure to be seen within the nerve which shows a speckled appearance in transverse section and linear streaks in longitudinal images which probably indicate something of the internal fascicular structure of the nerve. Nerves generally become more hypo-echoic (or darker) on ultrasound images at sites of injury but quantifying this as a number for measurement purposes is difficult. The absolute brightness of a pixel in an ultrasound image is not only determined by the tissue being imaged but also by the angle of incidence of the ultrasound beam on the tissue and the settings on the machine itself. It is easy to make a nerve look brighter or darker by tilting the transducer or twiddling the knobs on the scanner.
Nerve shape - attempts have been made to study the differences which are seen in the shape of the median nerve within the carpal tunnel. The most widely quoted of these is the 'flattening ratio' - the ratio between the largest and smallest diameters of the nerve.
Nerve vascularity - using the doppler facilities on modern scanners with settings chosen to detect blood flow in small blood vessels where flow rates are generally low it is possible to detect unusual increases in the blood supply of a tissue. This has been most widely used to detect inflammation in connective tissue but some workers are starting to use these methods to try and detect increased vascularity within the median nerve itself in CTS.
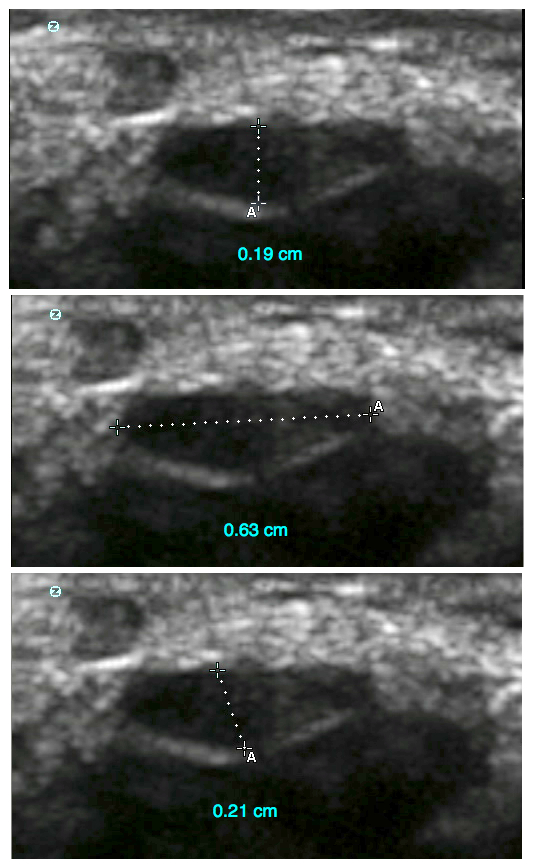
Subsynovial connective tissue thickness - Two recent studies (Ettema 2006, van Doesburg 2012) have suggested that it is possible to measure this accurately and reproducibly with ultrasound. This measurement seems to be pushing the capabilities of ultrasound imaging to the limit and it deserves looking at in a little more detail. The terminology is a little unclear in some of the anatomy literature so that it can be hard to know exactly what is meant by some authors when they are describing the structures within the carpal tunnel but these authors are using the term as follows:
The flexor tendons are cushioned and lubricated as they pass through the carpal tunnel by synovial 'sheaths'. The sheaths consist of bursae - fluid filled sacs a bit like rubber balloons with a little water in. In fact there is so little fluid in these bursae normally that the two layers of membrane forming the 'front' and the 'back' are opposed to one another. These bursae lie between the nerve and the tendons. Between the bursa and the tendons there is yet another layer of tissue and it is this layer which is described as the "subsynovial connective tissue". Thus, in this transverse image:

... we see that there is a gap between the nerve and the tendon (c-c) which is occupied by the epineurium (the outermost fibrous layer of the nerve), both layers of the bursa and the subsynovial connective tissue. There is possibly a further layer, between the epineurium and the bursa but in practice this seems to be no more than a potential space. In both of these studies, images were studied in the longitudinal view rather than this transverse one. Ettema et al studied cadaver hands and show an image where the FDS-III tendon lies directly adjacent to the flexor retinaculum so that there are no nerve related layers to confuse things. They were able to show a hyper-echoic layer above and below the tendon and demonstrate that it moved longitudinally at a different rate to the tendon when the finger was flexed using doppler imaging. They then measured the thinckness of this and found it to be about 0.6 - 0.7 mm. The same measurement was then made on an anatomical section and found to be about 0.8 - 0.9 mm.
van Doesburg et al made their measurements in live patients and control subjects and here the confusion begins. In their methods section they describe the SSCT layer as being a hypo-echoic, non-moving layer. However, further on in the same section they describe it as the "thin echogenic layer at the border of the tendon, between the median nerve and the FDS tendon" and their illustration certainly shows a measurement of a hyper-echoic structure. They found the thickness to be about 0.48 mm in controls and 0.62 mm in patients. One wonders if the first mention of a 'hypo-echoic' layer is a misprint.
This half-millimetre gap may well be widened in CTS patients but the idea that what is being measured is purely the subsynovial connective tissue layer seems a little unconvincing at present.
What is 'normal'?
Measured using the Sonosite M-turbo scanner used in Canterbury 84 normal hands show the following cross-sectional area distribution. All measurements were made using the highest frequency setting of the transducer and on 'zoomed in' images with manual tracing of the nerve outline just inside the hyperechoic margin:
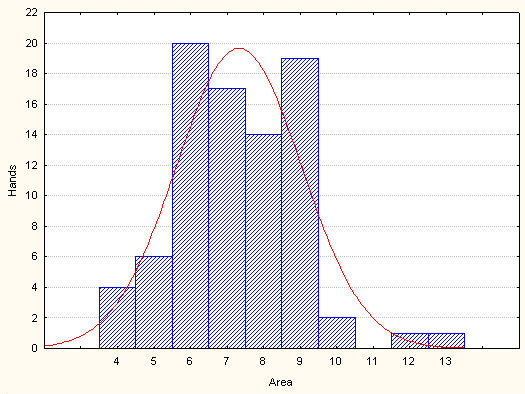
This is not a normal distribution and the limits of normality should not be determined using statistics dependent on such a distribution. For practical purposes the 95th Centile seems to be a useful upper limit of normal for now. 95% of observations fall below 10 mmsq, giving a 'normal' range of 4-9 mmsq. Nerves of 10 mmsq may be considered suspect.
The NEXT PAGE - illustrates the changes seen in CTS patients.
BACK - to the main ultrasound page
Revision date - 4th March 2012
