Ultrasound imaging after surgery
Expected changes in imaging after succesful surgery
There are as yet only a few studies of what the median nerves look like on imaging after surgery. There is reasonably good evidence that the nerve swelling reduces with successful treatment (Abicalaf 2007, Smidt 2008) and another study was able to show that the patients who did better after surgery had a larger decrease in size of their median nerves when comparing the pre and post-operative ultrasound images (Vogelin 2010), but it is not clear what proportion of nerves, if any, return to the normal range, how much improvement we should expect, or how quickly we should expect to see it after operation. We have seen asymptomatic patients many years after successful surgery who still have significant enlargement of their median nerves.
Another issue entirely is the assessment of failed carpal tunnel decompression. Naranjo et al, in their cohort of surgical patients, found that the decrease in CSA was similar overall in both the groups of patients with good results and the group with bad ones (Naranjo 2010) but there are anecdotal reports of ultrasound imaging being able to demonstrate incomplete section of the transverse carpal ligament when this is the reason for failure (Tan 2011).
Recurrent CTS after successful surgery
This 83 year old lady had bilateral carpal tunnel surgery in 2003 for a grade 5 right and grade 3 left CTS. The operations were entirely successful in relieving CTS symptoms until 2012 when she began to experience symptoms in the left hand which she recognised as similar to those she had had before surgery. The right hand remained asymptomatic, though she had sustained a Colles fracture on that side in the interim from which she had also made a good recovery, albeit with some deformity. Repeat nerve conduction studies showed a grade 1 right and grade 6 left CTS. The residual nerve conduction abnormality on the right side is not unusual after surgery for a severe CTS and the ultrasound imaging in the right hand showed a nerve cross sectional area of 14 mmsq - again probably a residual abnormality of little significance. The newly symptomatic left side however showed the following:

Figure 2
.jpg)
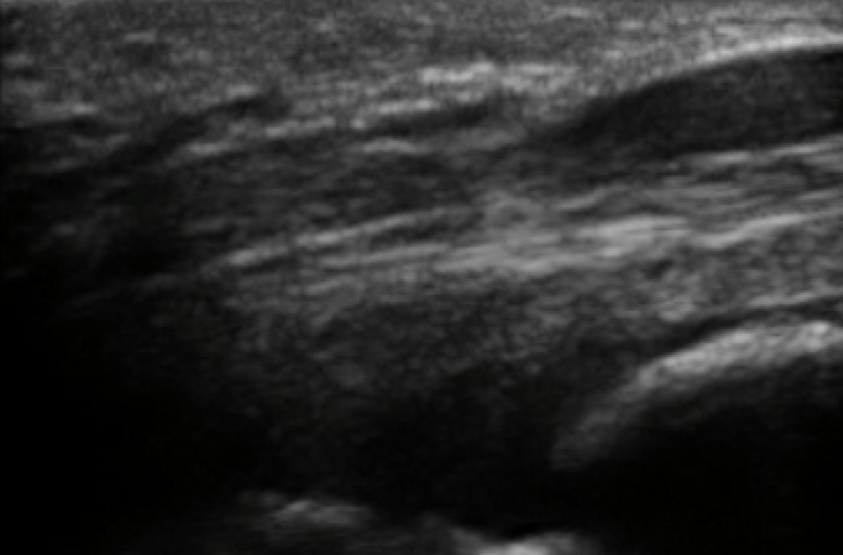
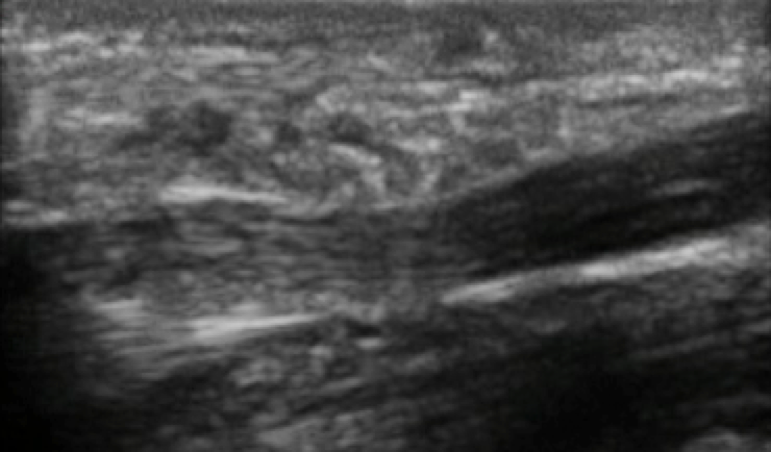
The left median nerve can be seen to be sharply indented by a dense fibrous stucture superficial to the nerve. The site of this band is just proximal to the wrist crease 2-3 cm proximal to the usual site of maximal compression in untreated carpal tunnel syndrome. The nerve shows marked enlargement just proximal to this indentation (27 mmsq) and is also enlarged distally being 11mmsq at the level of the hook of the hamate. Although it is impossible, in the absence of studies performed during the 8 years when she was free of symptoms, to tell for certain whether this constriction of the nerve is something which has developed anew, or is a residual fragment of transverse carpal ligament from the original operation, the clinical history strongly suggests that it is a new lesion and in any case it is clear that a surgical exploration proximal to the carpal tunnel will be required to release the nerve now.
Failure to fully section the transverse carpal ligament
This is the commonest reason for failure of carpal tunnel surgery to alleviate median nerve symptoms, probably acounting for half of all failures (Stutz 2006). When pre- and post-operative nerve conduction studies are available they usually show that nerve conduction has either stayed the same or deteriorated but in many cases pre-operative studies have not been done. The ultrasound imaging usually shows quite a prominent indentation in the nerve in the long-axis view and scanning along the nerve can confirm that this is not just a 'wiggle' in the course of the nerve taking it out of the plane of the scan. IN most cases this indentation extends along quite a short segment of the nerve, unlike the hourglass shape of the nerve in untreated CTS where the relative narrowing under the transverse carpal ligament extends over 2-3 cm and tends to have quite smooth transitions to the nerve on either side rather than an abrupt change in cross section. This is usually seen at the proximal (forearm) end of the incision rather than in mid-carpal tunnel or the palm.

In all of these three cases the nerve conduction studies were worse after surgery than they had been beforehand. There is some evidence that patients who have CTS in both hands and who have unsuccessful surgery in the first hand may be more likely to have a poor result from surgery on the second hand (Tang 2017). This may be because they are anatomically 'odd' in some way which makes it harder to get the surgery right, and if one hand is built in such a way as to make surgery difficult then it is quite likely that the other one wil be the same.
This patient had grade 3 bilateral CTS before surgery. She continued to have tingling in the right hand after surgery but nevertheless went on to have the left side operated two months later, also without marked improvement in symptoms. On re-testing two months after the second operation (at which time she felt the symptoms in both hands were worse than they had been before surgery) both sides were grade 6 on nerve conduction studies:
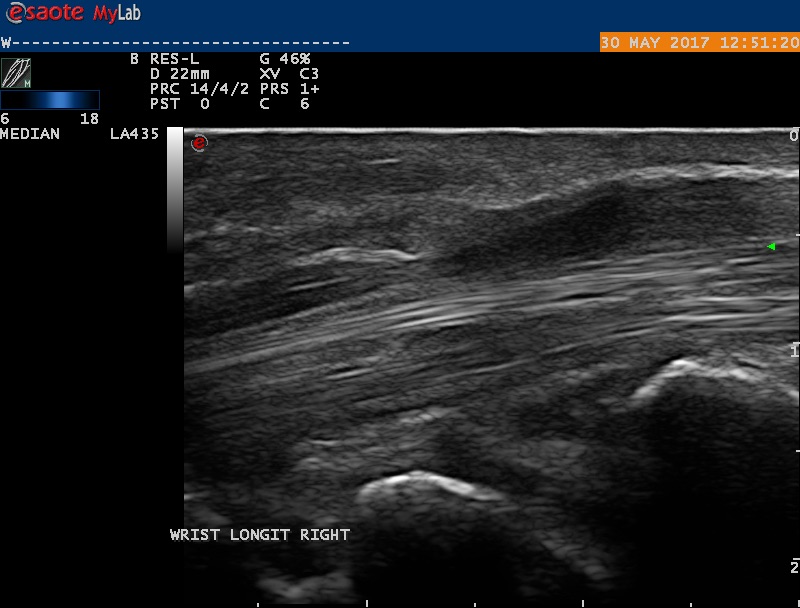

Although somewhat different in appearance on the two sides, both indicate probems somewhat proximal to the usual narrowest point of the carpal tunnel
Revision date - 11th September 2017
