Surgical Prognosis
The first thing the patient considering surgery wants to know is, will it work? The quick answer for carpal tunnel decompression is given here in the form of what over 6000 patients in East Kent, UK told me about the result of their carpal tunnel surgery when asked.
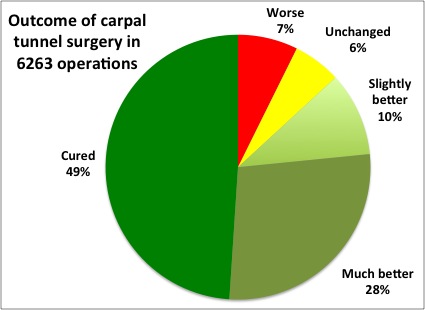
Note that only about half consider the hand to be 'as good as new' after the operation but three quarters are generally happy with the result and 87% are at least improved. That is the quick answer to how well does it work, at least as reported by the patients. We can however go quite a lot further in trying to predict which patients will do well and the rest of this page is devoted to a more detailed exploration of surgical prognosis. If you want to explore in detail much of what is known about factors influencing the outcome of carpal tunne surgery you can find much of it here. However there are two online calculators available which will combine many factors about your individual case to give you an estimate of the likely chances of success. One of them is on this website and is available from the "My CTS" page. The other one has been developed in the Netherlands and can be found online HERE in English. Note that when using the Dutch calculator, if you complete the various scoring questionnaires online you have to manually copy the scores back into the boxes on the main page for them, otherwise the calculate button generates an error message. I would be curious to know how East Kent patients get on with the Dutch calculator and how the predictions from the two systems compare.
What goes wrong with surgery?
The art of predicting the outcome of surgery is a difficult one. In respect of carpal tunnel syndrome, the majority of patients are very pleased with the outcome of their operation. However a few are not and it is those patients who actually feel that they have gained nothing from surgery - or are even worse off than before operation - who are of particular concern. If we could identify these before taking a knife to them that would be a huge improvement in care for carpal tunnel syndrome.
Failed carpal tunnel decompression, which is a convenient term, actually encompasses a variety of different clinical circumstances. The first thing to be clear about is that we are discussing patients who do not get the result they hoped for from their operation in the first place. There is a second group of patients whose operations are initially successful but in whom symptoms of CTS recur after a symptom free interval ranging from months to years. This is true ‘recurrent’ CTS and is actually comparatively rare but most published studies fail to distinguish between primary failure to relieve symptoms and later relapse after initial success. There are several papers using the term ‘recurrent CTS’ in their titles in which it is clear that most of the cases discussed are examples of primary failure to relieve the symptoms in the first place. The reasons for late relapse are very poorly understood and hard to study because it is such a rare occurrence. An example of what is probably a true recurrence is shown in the ultrasound pages. Here I am mostly concerned with primary failure.
Primary failure from the patient’s point of view means simply that whatever symptoms they have after surgery are as bad as, or worse than, those they had before operation. They may be the same symptoms or they may actually be completely different and this is probably the first thing to establish in analysing what has gone wrong. The main reasons for failure can be grouped thus:
a) Bad diagnosis - the original symptoms were not actually caused by median nerve entrapment at the wrist. This can occur whether or not there is a measurable nerve problem at the wrist - just because the nerve is showing signs of damage at the wrist it does not mean that the patient cannot actually have another problem which is the dominant cause of the symptoms. In such circumstances treatment directed at the carpal tunnel, predictably, does not solve the patient’s problem, and may in fact add to it by giving them the wrist problems discussed in the surgery section.
b) Bad surgery - the surgeon has injured something accidentally or failed to section the transverse carpal ligament fully. Victims of surgical trauma can include the median or ulnar nerves themselves, the recurrent motor branch of the median nerve, the palmar cutaneous branch of the median nerve, the palmar arch (blood vessels), the digital nerves and the flexor tendons.
c) Bad luck - some surgical complications are effectively random in nature - wound infections, complex regional pain syndrome, hypertrophic and painful scars, and persistent pain and weakness secondary to section of the transverse carpal ligament itself. One also has to include in this group when collecting outcome data some patients who simply develop another, completely different, hand problem during the period after surgery as it may not be possible to distinguish between problems caused by old and new pathology. Trigger digits and Dupuytren's contracture are both very common in patients with CTS and can confuse the overall pattern of symptoms.
d) Bad nerve - different types of nerve injury are known to have different prospects for recovery depending on the mechanism of injury, time since injury, site of injury, patient age etc. In the case of carpal tunnel syndrome it is demonstrably the case that patients with ‘advanced’ CTS shown by unrecordable median nerve responses on NCS, thenar atrophy and marked loss of sensation in the fingers, are less likely to be happy with the outcome of surgery than patients who do not show these features. It seems likely that these nerves may be effectively ‘beyond recovery’ and that, as is the case in a), operating on them in some cases not only has no effect on nerve function but simply adds the side effects of surgery to the patient’s overall problem. That is not to say that all such cases are hopeless however and good outcomes have been reported in some series of well selected patients. There are now enough studies of this topic that it is worth providing a dedicated section of the site which interested patients with very advanced CTS can read when considering surgery.
To some extent the distinction between b) and c) is artificial - all are technically surgical complications but the things categorised under b) really SHOULD not happen. In a legalistic climate one could argue that these are the things which might lead one to sue the surgeon though I am not aware of any UK case of a patient successfully taking a surgeon to court because their carpal tunnel decompression was a failure - if there are any I would be curious to hear about them.
How can complications and poor outcomes be predicted and/or avoided?
Bad diagnosis can obviously be reduced by meticulous attention to detail by an experienced clinician aided as necessary by diagnostic tests and I believe that this factor is a significant one in the achievement of the very high success rates reported by some surgeons. If one further limits surgery to only cases in which one is very certain of the diagnosis, and does not operate on people with equivocal clinical features, then it is possible to select a patient population for surgery in whom bad diagnosis, as a cause for surgical failure, is almost non-existent. There are people however in whom the diagnosis is somewhat uncertain, even after exhaustive investigation, and if one operates on these cases one has to accept that the success rate will be lower, even though some will be dramatically improved.
Bad surgery is a direct consequence of poor surgical expertise. Unfortunately, surgical expertise is largely acquired through practice. Every hand surgeon, however well trained and supervised, at some point has to perform their first solo carpal tunnel decompression. In the UK a good many carpal tunnel decompressions are performed by surgeons in training (under supervision), precisely because this is seen as a simple operation. Thus, if you want the best chance of a good result from carpal tunnel surgery you go to a surgeon who has done lots of them and already demonstrated a high success rate. Unfortunately you may not have much choice and when you do have a choice data of any quality on the number of procedures carried out by different surgeons and their clinical results will rarely be available - even for such a common procedure as carpal tunnel decompression. You can see from the data shown here that measuring surgical outcome is not so simple as just counting the satisfied patients by surgeon - someone who sees all the grade 6 cases because they are particularly good at hand surgery is actually going to have rather poor looking results. Even in my own area where we make attempts to track the outcomes of carpal tunnel surgery in detail I only have comparative data of a quality which allows me to comment on which people are best at it for three out of some thirty or so surgeons who carry out the operation.
Bad luck - something which all of this group have in common is that they are unpredictable. No amount of pre-surgical information gathering is going to be able predict that Mrs X is going to fall and fracture the wrist badly 2 days after surgery, nor that Mr Y will develop complex regional pain syndrome (at least given our current level of understanding of these conditions)
Bad nerve - At present the only wholly objective measure of median nerve function available which allows one to express the severity of the injury in numerical terms is the nerve conduction study. Imaging methods can quantify the nerve swelling seen in CTS but as yet this has not been clearly linked to prognosis whereas a considerable amount of (sometimes conflicting) data is available to tell us how pre-operative NCS relate to surgical outcome. Some clinical examination findings are known to correlate with severely abnormal nerve conduction studies and with a relatively poor prognosis but these are harder to quantify. Subjective measures of symptom severity such as the symptom severity subscale of the Boston CTS questionnaire do not correlate with surgical outcome but high scores on the functional impairment subscale are associated with poorer outcomes because they are indicators of severely impaired nerve function.
For the present, the best indicator of prognosis in respect of ‘bad nerve’ is the nerve conduction study. Even in this field however there is no agreement on exactly how to measure CTS severity on nerve conduction studies, a problem largely created by the plethora of different neurophysiological testing methods for CTS. It is usual to make more than one measurement of median nerve function when carrying out nerve conduction studies and one may find differing degrees of abnormality in the different tests. How one resolves a situation where one test indicates a moderately severe CTS while another is normal into an overall measure of severity provides scope for considerable differences of opinion. The solution adopted in my own department is the Canterbury NCS scale for CTS and we have studied the way in which pre-operative test results expressed on this scale relate to the patient’s opinion of the outcome of surgery in over 5000 operations. The findings are summarised in this graph. We asked patients to give an overall opinion of the success of their surgery using a global outcome scale.
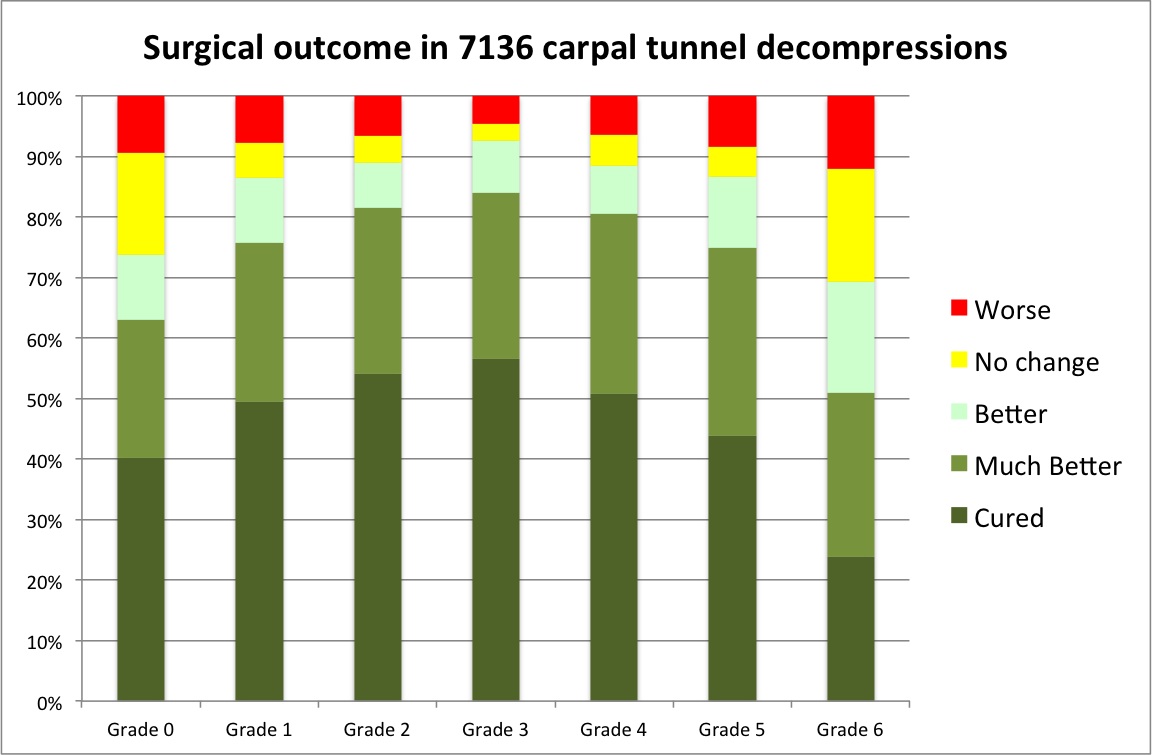
It is obvious that there is a markedly reduced chance of a really good subjective outcome after surgery if the pre-operative NCS show grade 6 CTS and that in fact the chances of a good result fall from grade 3 upwards. It is a curious observation however that, at the other end of the scale, grade 1 and 2 cases are also less likely to do really well surgically. My own interpretation of this is that it largely represents misdiagnosis and that, the milder the physiological impairment of the median nerve, the more likely it is that some other pathology is actually contributing to the patient’s symptoms. Other workers who have looked at NCS as a predictor of surgical outcomes have obtained contradictory results, many of which can be explained by looking at this graph and the patient population studied. Choosing a population of generally mildly affected patients leads to a situation in which more severe physiological abnormalities are found to correlate with better surgical outcomes. Selecting a group of patients with moderate to severe CTS (usually the population found in surgical clinics) gives exactly the opposite result with more severe physiology being correlated with a worse surgical outlook. Using an inadequate neurophysiological grading scheme such as one which effectively lumps together grades 1-2 and 3-6 leads to a situation in which there seems to be no difference in outcome between the milder cases and the more severe ones, especially in small studies with limited statistical power.
Other Prognostic Factors
The literature relating to surgical prognosis for CTS is extensive and confusing and some pointers to it follow:
MOTOR DEFICIT - 6 out of nine studies have found the existence of demonstrable weakness of the median innervated muscles in the hand to be a poor prognostic factor for surgical outcome. The other three studies found no effect. This clinical finding is simply a marker for advanced carpal tunnel syndrome with significant nerve damage.
IMPAIRED SENSATION - usually demonstrated in CTS as impaired 2-point discrimination (the ability to detect that two nearby simultaneous pin-pricks are two points rather than one - a test which can be made quantitative by varying the distance between the two points). Also sometimes done with von Frey hairs which are calibrated fibres which apply a known force to the skin when applied so that they just bend. Two out of four studies have found demonstrable sensory impairment to be a poor prognostic factor
PREDISPOSING CONDITIONS - 7 out of ten studies have found poorer outcomes in patients with other coincident conditions, including both disorders which are thought to be causative for the CTS and purely incidental musculoskeletal or other problems. There are however studies of, for example diabetes (see below), or patients with generalised neuropathy, which suggest that treatment of CTS in these cases is just as successful as in ordinary, idiopathic cases.
DIABETES - The interaction between carpal tunnel syndrome and diabetes is complicated. It is generally believed that CTS is commoner in diabetic individuals, whether or not there are other diabetic nerve complications. Diabetic patients are prone to a complex of hand problems including Duputren's contracture, trigger digits and stiff fingers - sometimes termed 'diabetic hand' (See the page - The Triad). It also appears to be the case that diabetic patients get slightly different symptoms from CTS compared to non-diabetic patients. Several studies have found that diabetic patients tend to present with more severe neurophysiological abnormalities, eg (Jenkins 2012), so multivariate statistics are required to determine whether diabetes itself has an effect on the outcome of surgery. The existing data is contradictory and as usual many studies are small with inadequate power to do the necessary statistics. The topic has been the subject of a recent review in the Journal of Hand surgery (Brown 2011). To illustrate the difficulty, consider the following ten papers about 8 study populations:
Al-Quattan et al (1994) studied 20 hands/operations in 15 diabetic patients and obtained good or excellent outcomes in 8 hands, intermediate results in 7 and poor in 5. All of the poor results had had minimal or no evidence of CTS on pre-operative nerve conduction studies. (Haupt 1993) found poorer outcomes in diabetic patients (86 hands in 60 patients, only 10 diabetic) whereas (Choi 1998) did not (254 hands in 154 patients, 19 diabetic). These two studies however included relatively few diabetic patients. Another small study (Thomsen 2009) compared 35 diabetic patients with 31 non-diabetic patients having carpal tunnel surgery. Results were identical in the two groups in most respects at 1 year after surgery, most importantly overall patient satisfaction, but the diabetic patients reported less improvement in the curious symptom of 'cold intolerance' - not a symptom of CTS which is widely recognised or studied. Some multivariate analysis was attempted but the sample size was probably too small for this to be very useful. These authors reported the neurophysiological findings in their patients in a separate paper (Thomsen 2010) showing more severe baseline nerve conduction abnormalities in the diabetic patients but similar degrees of improvement with surgery. Finally they have gone on to report the 5-year outcomes (Thomsen 2014), again finding no differences between the two study groups, even the difference in cold intolerance having largely resolved. This being Sweden they had a remarkably high 5-year follow-up rate, 86% of patients returning for a follow-up examination and 95% returning the Boston questionnaire. The largest of these old studies (Pagnanelli 1997) compared 149 diabetic patients with 200 control subjects with CTS and provided overall patient opinions of the outcome with an 84% success rate in the diabetic patients as a whole, 81% in the insulin dependent patients and 90% in the non-diabetic cases. (Zyluk 2013) compared 41 diabetic and 345 non-diabetic subjects assessing the outcome at 6 months with Boston/Levine SSS/FSS scores, grip and pinch strength measurements and Semmes Weinstein monofilament testing for sensation. They found no significant difference between diabetic and non-diabetic patients but the statistical analysis here was unsophisticated. (Ozkul 2002) looked at only 22 diabetic and 25 non-diabetic patients (60 hands operated) and looked at patient reported outcomes at 1 year, this time using the global symptom score (GSS). The diabetic group improved from 27.6 to 17.0 while the non-diabetic group improved from 27.2 to 5.9 - a significantly better result in the non-diabetic subjects but again this is a very small study of a single variable. The Italian CTS study group has also looked at the outcomes of surgery in diabetes (Mondelli 2004), studying the outcome in 24 diabetic patients in compariosn to 72 age/sex matched controls at 6 months after surgery. No significant differences in outcome assessed using the Boston/Levine SSS/FSS were found.
If the reader is confused at the end, this is hardly surprising with a such a disparate batch of conclusions. What probably can be read into these studies is that, if diabetes is a poor prognostic factor, it is not a very important one, otherwise even these small studies would come to more of a consensus view.
The Dunfermeline group have published one of the best and largest studies, involving 1654 patients of whom 176 were diabetic (either type I or type II diabetes). The analysis was performed for the worst affected hand in each patient. The diabetic patients were older, had higher body mass index, and had more severe nerve conduction abnormalities. Outcomes were assessed as the mean change in QuickDASH score one year after surgery. The QuickDASH score can range from 0 to 100 and it is considered that a change of 8 units is clinically meaningful. In the raw results the diabetic patients improved from a mean score of 59.2 to 27.5 while the non-diabetic patient simproved from 55.9 to 20. They were able to carry out a partial multivariate analysis allowing for difference in age and gender (women for example having poorer rates of improvement). At the end of this they concluded that the diabetic group had poorer QuickDASH scores both before and after surgery but similar amounts of change in the QuickDASH score. They were not however able to take into account the difference in nerve conduction results between the groups. (Jenkins 2012)
In data from our own patients in Canterbury we are currently studying a series of 3332 operations in 2671 patients (with a further 885 operations being used to prospectively test our models). 405 of these operations were carried out in diabetic patients. Non-diabetic patients do slightly better overall with a 75% success rate compared to 71% for diabetic patients. We are currently analysing this as one factor in a complex multivariate model.
RESPONSE TO INJECTION - Two studies have reported better outcomes in patients who have previously shown a good, if temporary, response to local steroid injection (Edgell 2003) (Kulick 1986)
AGE- Four out of seven studies have reported poorer outcomes in older patients.
DURATION OF SYMPTOMS - Six out of ten studies have reported a longer duration of symptoms before operation to be predictive of a poorer outcome.
GENDER - Better results have been reported in both males and females with no overall consensus.
IMPAIRED ACTIVITIES OF DAILY LIVING - Formal tools exist for evaluating the impact of disease on one’s ability to carry out ordinary daily tasks. In two studies, scores on such assessments indicating greater impairment have been correlated with poorer surgical outcome. Again this is largely a proxy measure for advanced CTS with a good deal of nerve damage. The functional impairment subscale of the Boston CTS severity questionnaire used here in one such assessment tool.
STRENUOUS MANUAL OCCUPATION - Six out of seven studies have reported poorer outcomes in patients with heavy manual occupations.
SMOKING - One study has reported poorer outcomes in smokers.
ALCOHOL - The same study also reported poorer outcomes in drinkers - both tobacco and alcohol use may be markers of general health status rather than being specifically implicated in CTS.
COMPENSATION - In most American studies patients who are the subject of an industrial injury compensation claim for their CTS have a worse prognosis then those who are not involved in such a claim. In one study the outlook was particularly bad specifically in those patients in whom a lawyer was involved (Katz 2001)!
What to do when surgery fails
A significant number of patients now make their way to me because they have had surgery for CTS and have not improved to the extent they were expecting. This is a sufficiently difficult problem that I have given it a dedicated page on this site.
Revision date - 1tth January 2022
