Prognosis for non-surgical options
A little information is starting to emerge about how to predict what will happen to CTS symptoms if you either do nothing, or attempt non-surgical treatment. We are not concerned here so much with the raw success rates reported in trials of different treatments but with factors which help to predict which patients will, or will not, respond well to any one given treatment. Non-surgical treatments are often used in combination so it can be hard to separate out individual effects but some information is currently available for the following options:
Do nothing
There are very few studies of untreated CTS to tell us what is likely to happen if we do not intervene. There are difficulties in performing such studies because it is not considered ethical to randomly allocate patients to no treatment when an effective treatment is available. The best available information comes from a study of 196 patients (274 involved hands) who volunteered to forego treament for a while (Padua 2001). About one fifth of these patients improved. Factors associated with spontaneous improvement were:
Shorter duration of symptoms
Younger age
Unilateral symptoms
A negative Phalen's test
A second study from Japan looked at 257 patients (Futami 1997) but it is not clear why these were not actively treated. They are all described as either right or left sided CTS with no mention of bilateral cases and a substantial number were pregnant. No multivariate analysis of the outcomes was performed but in single variable analyses the natural remission rates were higher in:
Younger patients
Pregnant patients
Females
As the pregnant patients will have been concentrated in females (obviously) and younger patients the analyses of outcome for these factors would have been better done excluding the pregnant patients. The same authors published an earlier study in which 155 of 203 patients were followed up without treatment. 61 of these were bilateral. 55 patients reported complete remission of symptoms (Futami 1992). It is not clear whether the1997 study included this earlier cohort of patients and was simply an extended verion of the same study.
Overall it appears that doing nothing may be a viable strategy in some patients - definitely in pregnancy and probably in younger patients with a short history and unilateral symptoms.
Neutral angle wrist splinting
Gerritsen et al (2003) analysed data from their trial of splinting vs surgery to see if they could find factors which predicted which patients would gain long-term (1 year) relief from splinting only without having to resort to other treatments. They found only two factors which predicted success with splinting
- A short duration of symptoms before treatment (less than 1 year)
- A lower score on a subjective measurement of the severity of tingling at night (6 or less on a scale ranging from 0-no symptoms to 10-very severe symptoms)
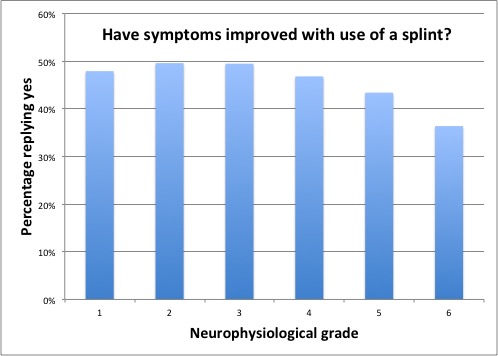
In data from Canterbury patients, those with more severe grades on NCS are somewhat less likely to report benefit from splinting as are those with higher SSS and FSS scores, larger nerves on ultrasound imaging, no history of night waking or constant symptoms.
Local steroid injection
Several of the existing studies of steroid injection for CTS have tried to identify which patients had better results. They are summarised in the table below. All of these studies looked for prognostic factors which predicted prolonged remission after injection, not the initial response which they all agree is quite good for most patients. The item on which there is most agreement is that patients with a shorter history (Hx) of CTS symptoms tend to do better (4 out of 7 studies which looked at that variable). 'Yes' in a cell indicates that that variable was studied and was associated with a better outcome. 'No' indicates a variable which was studied and had no correlation with outcome. Blank cells indicate a variable which was not looked at in that study.
Note the contradictory findings on age with one study finding older patients doing better and another finding that younger patients had better results. Most studies seem to find that age has no effect.
| Study | Author | Gelberman 1980 | Kaplan 1990 | Weiss 1994 | Irwin 1996 | Graham 2004 | Ollivere 2009 | Meys 2011 | Visser 2012 |
Blazar 2015 |
| Steroid | TC | ??? | BM | HC | BM | ??? | MP | MP | TC | |
| Dose | 30 | ??? | 6 | 100 | 3x3 | ??? | 40 | 40 | 10 | |
| With Splint | Yes | Yes | Yes | No | Yes | Yes | No | No | No | |
| Follow-up | 18m | 15m | 12m | 12m | 12m | 2y | 12m | 18m | 12m | |
| Predictors | ShortHx | Yes | Yes | No | Yes | No | Yes | No | ||
| Lower NCS grade | Yes | No | Yes | No | ||||||
| Sex (female) | No | Yes | No | No | ||||||
| Side (dominant) | No | No | ||||||||
| Lower SSS | Yes | Yes | Yes | No | Yes | |||||
| Smaller CSA | Yes | |||||||||
| Age | Yes (<50) | Yes (>40) | No | No | No | |||||
| Lower FSS | Yes | No | ||||||||
| Less P+N | Yes | No | ||||||||
| Less Numb | Yes | No | ||||||||
| Less Pain | No | |||||||||
| Normal Sensation | Yes | |||||||||
| No Weakness | Yes | No | ||||||||
| Phalen >30s | Yes | No | ||||||||
| Workers comp | No | |||||||||
| Bilateral | No | No | ||||||||
| Non-Diabetic | Yes | |||||||||
| Osteoarthritis | No | |||||||||
| Bilateral inject | No | |||||||||
| No Sten Flex Tendonitis | Yes | No |
Steroid Key: TC=Triamcinolone, BM=Betamethasone, HC=Hydrocortisone, MP=Methylprednisolone
Different steroids have different potencies - strength of biological effect per mg. For commonly injected steroids approximately equivalent doses are as follows:
Hydrocortisone - 100mg (Short acting)
Prednisolone - 25mg (Intermediate)
Methylprednisolone - 20mg (Intermediate)
Triamcinolone - 20mg (Intermediate)
Paramethasone - 10mg (Long acting)
Dexamethasone - 4mg (Long acting)
Betamethasone - 3.3mg (Long acting)
Abbreviations that may need explanation - SSS and FSS are the subjective severity scores from the Boston questionnaire. P+N=Pins and Needles severity measured on a visual analog scale. CSA is the median nerve cross sectional area measured on ultrasound.
The recent study by Blazar 2015 deserves one or two extra comments. These authors allowed the injecting doctors to use either 10mg triamcinolone or 4mg dexamethsaone. They think that these doses are equivalent potency whereas the figures I have found suggest that the 4mg dexamethasone dose is about twice as potent as 10mg triamcinolone. They found no diference between the two injections however. They do not tell us how many hands received each type of injection and probably did not have enough hands in the study to detect a modest difference between these two low doses. Around 40% of their study hands were free of symptoms at one year and 60% had required no further intervention. This paper includes a useful table summarising 22 previous studies which have reported outcome after injection but the patient populations, outcome measures, follow-up periods and interventions (dose of steroid +/1 other things in parallel) vary so much that it is impossible to calculate any sensible overall representative figures from these studies.
In the study by Ollivere 2009 the SSS score was a better predictor of outcome than the FSS score. 14 out of 58 cases(24%) responded so well to the conservative treatment in three months that surgery was not felt necessary and all of these patients apparently remained well 2 years later. All but two of the conservatively treated patients had one steroid injection as part of their treatment programme but we are not told the steroid or dose. 67% of patients with a Boston symptom severity score of 2.5 or less responded well to non-surgical treatment while 89% of patients with a score of greater than 2.5 required surgery. You can work out your own Boston severity score by completing the questionnaire on this site.
The study by Graham 2004 was unusual. They began with 3mg of betamethasone and then reviewed the patient after 3 weeks, at which point they gave a further 3mg if there were still symptoms, followed by a further 3mg at 6 weeks if necessary... after which they gave up and operated if there was still a significant problem.
The study by Kaplan 1990 is problematic and its results should be taken with a pinch of salt. 331 hands in 229 patients were studied which makes it quite a large study, but they were mostly treated with splints and non-steroidal anti-inflammatory drugs. Only 16% of the patients received a steroid injection and we are not told which steroid or the dose used. 27% of the patients were given oral steroids but we are not told whether there was any overlap with those given injections. The outcomes for the groups given steroids are not described separately from the whole group so this study only gives one a very broad brush view of non-surgical treatment and probably says little about steroid injection in particular. One of their poor prognostic indicators was the presence of 'Stenosing Flexor Tenosynovitis' but they do not specify how this diagnosis was made, and indeed their diagnosis of CTS may have been uncertain in some cases as they did not use NCS for confirmation.
Looking at the initial responses to first injections in Canterbury in 1566 injections it is apparent that there is some variation in success rate relating to the pre-injection severity of the nerve conduction abnormalities which follows a similar pattern to that seen with surgical treatment. Note that there is no grade 6 column in this graph because we do not inject enough grade 6 cases to obtain a statistically valid view of the outcome. The markedly lower success rate in grade 0 (normal NCS) cases is probably a result of us using steroid injection in these patients as a further 'test' for carpal tunnel syndrome when the diagnosis seems especially uncertain.
.jpg)
Patients who report themselves 'worse' after steroid injection are mostly suffering from worsening of their CTS because they have not responded to steroids. Adverse effects from all of these non-surgical treatments are so rare/mild that no predictive factors have been identified.
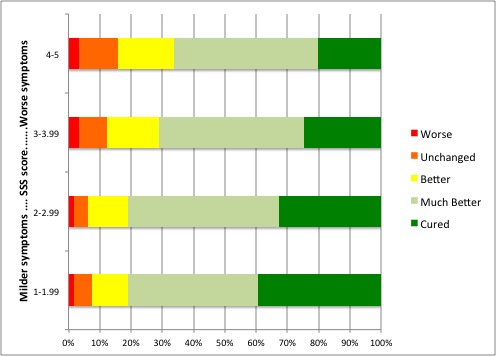
Data from Canterbury suggests that patients with more severe symptoms are less likely to respond well to injection. The following graph shows the patient reported outcome about 6 weeks after injection for 1600 hands (First injection performed in each patient). We have divided the patients by pre-injection Boston SSS score into 4 groups - the score can range from 1 to 5.
If the patient does respond well to steroid injection to begin with, then predicting how long they will remain well is even more difficult but some clues are given by the existing literature summarised above.
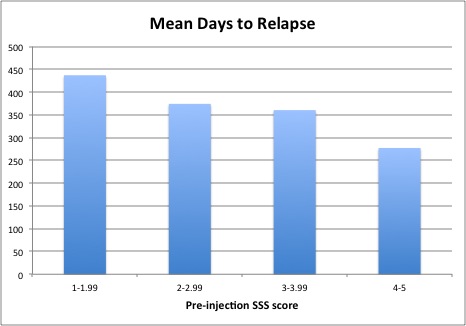
A very preliminary analysis of Canterbury data suggests that the pre-injection SSS score predicts not only the initial response rate to injection but also the length of remission. The following graph shows the average time to relapse for the same four categories of pre-injection SSS. It is important to note however that this data relates only to the 640 patients who we know have relapsed after an initial good response. It takes no account of those patients who are, so far as we know, still in remission and much work remains to be done on this topic.
Surgery is a more complex issue and has it's own page
Revision date - 2nd May 2016
