Carpal Tunnel Surgery
This page has the following sections:
Description of carpal tunnel surgery
Problems with surgery and complications
Speed of recovery after surgery
Long-term outcome - does CTS ever come back after surgery?
Description - Surgery has been the mainstay of CTS treatment since the 1950s and has received the lions share of scientific attention with endless publications devoted to minor variations of surgical technique. The principle is very simple - the tunnel is constricting the nerve so make the tunnel bigger. In practice the simplest way to achieve this is by cutting the transverse carpal ligament, effectively converting the carpal ‘tunnel’ into a carpal ‘trench’ - albeit one still covered over by skin and subcutaneous tissue. More complex procedures in which the ligament is lengthened rather than merely cut do not seem to be any more or less effective and have not been widely adopted and there are now generally two broad approaches to how to do it which may be termed ‘from the outside’ and ‘from the inside’.
The first is the obvious and traditional approach - make an incision over the carpal tunnel area, identify the ligament and, being careful to protect the nerve, its branches and other vital structures in the area, cut it. The incision is a small one at the heel of the hand - an operative photograph appears on a separate page so that people do not come across graphic illustrations of surgery without warning.
The second approach is the province of ‘keyhole surgery’ - essentially an instrument of some kind is inserted into the carpal tunnel and the cut to the transverse carpal ligament is made from the inside out. (Purists might argue that in both methods the cut is actually made from end to end of the tunnel not from either inside or outside but this does not invalidate the overall concept)
There are many small variations on both techniques which are not worth listing here. This is not a manual for surgery. The bottom line is that the long term results of the two approaches are indistinguishable, the only measurable difference between them being that recovery is slightly faster after keyhole surgery, by a matter of a few days. Unless you are very concerned about time taken to return to work it is more important that you find a good surgeon who is happy with the method that he or she uses than it is to choose a particular surgical method. The issue of return to work after surgery is addressed below.
One of our patients has provided us with a very vivid account of a fairly average operation and recovery period
Is surgery always necessary? Although there are a few surgeons who seem to believe that every patient who presents with CTS (with the possible exception of pregnant ones) will eventually need surgery at some point, the case for this is far from proven. There are very few long-term studies of patients with CTS who have not been treated surgically. One study attempted to analyse the records of 600 patients with CTS over a 15 year period (DeStefano 1997). They were able to trace records for 425 and found that 198 (46%) had had surgery which suggests that there are significant numbers of people who are not operated. In George Phalen's original case series of CTS patients (Phalen 1972) only 127/497 (25%) of hands which had initially been treated non-surgically had been operated by the time of follow-up but the length of follow-up in this case is not certain. Anecdotal reports and some limited studies of untreated CTS (Padua 2001) suggest that at least some patients may recover without any active medical intervention. It has been suggested (Muhlau 1984) that it is a good idea to wait 6 months after diagnosis before recommending surgery unless there are particular reasons to operate. In our own study of patients followed up for 8 years after an initial injection, only 41% had proceeded to surgery, though many had had further injections (Hameso 2017).
New variations on surgery - Surgeons are inventive people and in recent years have come up with several alternative ideas for dealing with the transverse carpal ligament including weakening it with 'multiple needle fenestration' (Malone 2010), stretching it with 'balloon carpal tunnel-plasty' (Berger 2006) and cutting it with a piece of sophisticated string under ultrasound control (Guo 2014). None of these newer techniques have been extensively studied and they must all be considered experimental for the present.
Problems with surgery - It cannot be denied that surgery for carpal tunnel syndrome technically constitutes a deliberate injury to the ‘natural’ structure of the wrist. After all we presumably have a transverse carpal ligament because it serves some biological function and one might wonder what the effect of cutting it might be in a normal wrist. In fact the transverse carpal ligament seems to perform two tasks.
Firstly it holds down the flexor tendons at the wrist and forms a pulley for them to act around when they flex the fingers. Without it, when the wrist is flexed and a power grip is used the tendons can be seen to be more prominent than usual at the wrist - a phenomenon known as ‘bowstringing’. The change to the mechanical action of the flexor tendons seems to result in slight loss of grip strength and when this is measured objectively hands after carpal tunnel surgery are, on average, about 2% weaker. Note that carpal tunnel syndrome itself does not usually have a profound impact on grip strength as this movement is performed mainly by the forearm muscles which are not affected by CTS. People do drop things a lot when suffering from CTS but this is probably not directly a result of weakness of grip.
Secondly the transverse carpal ligament helps to hold the wrist bones in a particular physical configuration. The bony structure of the wrist (the carpus) includes 8 small bones which lie between the ends of the long forearm bones (the radius and ulna) and the small bones of the hand (the metacarpals). It is this complex bony structure that gives the wrist its remarkable flexibility but it also means that there are a very large number of joints between the various bones which actually comprise the structure which we rather simplistically think of as the ‘wrist joint’. The carpal bones are arranged roughly in two rows of four each with each row taking up an ‘arch’ shape which is convex towards the back of the hand and concave towards the palm. The carpal tunnel nestles inside this arch and the transverse carpal ligament spans the gap between the two sides. When it is cut the arch tends to ‘open out’ and the spatial relationship between all these small bones changes slightly, placing unaccustomed stresses on the ligaments which hold them all together.
These changes are an unavoidable consequence of correctly performed carpal tunnel decompression and thus cannot be considered ‘complications’ of surgery which can be avoided by good technique. Mostly they do not cause post-operative symptoms which are worse than the original problem of having the nerve trapped but some patients are troubled by persistent weakness and wrist pain after surgery.
Two other difficulties are peculiar to carpal tunnel surgery and are in some ways inter-related. The heel of the hand gets a lot of everyday ‘wear and tear’ in normal daily activities and is not an ideal place to have a surgical scar which may become tender or hypertrophied with excessive scar tissue. The traditional open operation thus leaves a scar in an unfortunate place and this is one reason for the development of ‘keyhole’ approaches which avoid this. Another consequence however is that surgeons are under some pressure to keep the incision as short as possible and as a result their view of the transverse carpal ligament at surgery may not be as good as they would wish. It is therefore not too surprising that in some cases they do not manage to cut all of the ligament but leave a portion of it still compressing the median nerve - usually at the forearm end of the tunnel rather than the hand end.
In addition to this, carpal tunnel surgery is an operation like any other and is vulnerable to the same kinds of surgical risk which affect any other operations. Surgeons unfortunately do sometimes cut, stretch or compress structures which they should not and some patients will get wound infections or vascular complications which can make more of a mess of the hand than the original CTS. A few unfortunate patients are afflicted by a poorly understood condition called complex regional pain syndrome (old name reflex sympathetic dystrophy) which can follow any injury to a limb. A full discussion of this difficult condition is outside the scope of this site but a good starting point for information about it is the NHS choices website.
The bottom line is that not all patients are satisfied with the outcome of their carpal tunnel operation and in my own area about 8% of all operated patients consider their hand to be worse after surgery than it was beforehand. (people who have seen me may remember that I usually quote a figure of 5% failure for surgery - this is because some failures are predictable, at least in a statistical sense and I am modifying the figures to the particular circumstances of the patients that I personally am recommending surgery for - see elsewhere for much more on surgical prognosis). Although this is considered a successful operation by general surgical standards, and most patients are undoubtedly very satisfied with the results it is also true that a few of the worst affected patients have their lives ruined by the consequences of carpal tunnel surgery and it is not a procedure to be undertaken lightly.
In the many published series of carpal tunnel operations there is considerable variation in the reported surgical success rate and it appears that some surgeons are able, presumably through a combination of good patient selection and surgical expertise, to achieve better results than others (Bland 2007). I have spent many years exploring the factors which might influence surgical outcomes for CTS and what I have discovered so far is covered in the section on surgical prognosis.
Speed of recovery after surgery
A very frequent question from patients on the net is "how quickly should I be expecting my symptoms to improve now that I've had the operation" and the corrollary - "I had the operation 'x' weeks ago and it still hurts - is this right?". Some patients are told exactly what to expect by their surgeons before the operation but many are only told rather vaguely. When relief of symptoms is not prompt many surgeons seem inclined to adopt a 'wait and see' approach which implies that many patients do get better eventually even if they have problems weeks or months after surgery. There is surprisingly little good quality scientific data to allow us to say what the average patient should expect in the few weeks after surgery but a recent paper has provided some very useful data on how subjective symptoms change after the operation (Kronlage 2015). These authors tracked the SSS score (how bad the symptoms of CTS feel to the patient overall) for a year after surgery in 95 patients:
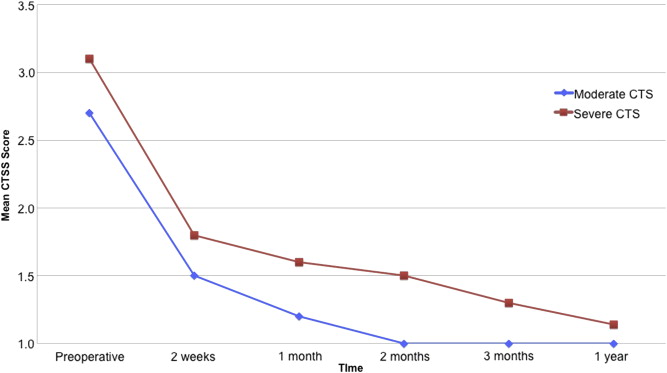
(Figure 1 - CTSS total scores in patients with moderate and severe CTS - Reproduced from The Journal of Hand Surgery, Vol 40, Issue 3; "The benefit of Carpal Tunnel Release in Patients With Electrophysiologically Moderate and Severe Disease" Pages 438-444.e1, Copyright 2015, with permission from Elsevier)
It is clear that the average patient is feeling much better by even two weeks after surgery. Even more interesting is that it documents the difference in recovery if the subjects have more severe nerve conduction study abnormalities before surgery. In this study the 'severe' group is those with an absent sensory nerve action potential - in Canterbury terms that is grade 4-6 patients, while the 'mild' group is grades 1-3. The 'severe' group have a more prolonged recovery and some do not reach the basline at all (a score of 1 on the SSS = no symptoms) whereas all of the mild cases had recovered fully by 2 months. Patients in grades 4 and above can therefore be told that they can expect to keep improving for quite a long time, but conversely even those patients should be feeling somewhat better 2 weeks after surgery and the lack of any improvement is a cause for concern. A larger study looking at more subdivisions of severity would be desirable as it is possible that there may be considerable variation in the recovery profiles between grades 4,5 and 6.
Return to work after surgery
For patients in employment a frequent question is “ how long will I be off work?” Although the topic has been quite extensively documented it turns out to be a difficult question to answer. Much of the existing literature on surgical treatment for CTS comparing different variations of surgery, for example traditional open surgery vs one of the endoscopic methods, uses the time to return to work after surgery as one measure of outcome, and it has been fairly convincingly shown that return to work times are a couple of days shorter for endoscopic than for open surgery. What this finding tends to conceal is the fact that other factors are much more important than the type of surgery in determining the length of time off work. It should be obvious, when you think about it, that the type of work involved is going to be a major determinant of time off, and indeed this proves to be so.
A large study in France (Parot-Schinkel 2011), reported a median time to return to work after carpal tunnel surgery of 60 days and found that type of occupation was the strongest determinant of how long the patient would be off, with manual 'blue-collar' workers requiring most time off. One american study (Katz 1997) found that 23% of patients still had not returned to work 6 months after surgery. In contrast in Denmark the mean sick leave after surgery was 20 days and only 3% of patients were still unable to work 3 months after surgery (Hansen 2009). In Norway the median time off was 7 weeks with 10% unable to return to work at all (Bekkelund 2001).
(Cowan 2012) looked at other factors influencing return to work times and found that desk based workers returned to modified work an average of 6.7 days after surgery and to normal work after an average of 9.5 days, though there was considerable variability. On the other hand, those subjects with non-desk based jobs required average times of 17.7 and 29.5 days to return to modified and normal work respectively.
A further interesting observation from this paper is that the pre-operative expectations and needs of the patient tend to be borne out in practice. People who expected to be off for longer tended to be right and people who expressed a pre-operative desire to get back to work quickly tended to do so. All of the patients in this study had essentially the same operation and the same pre-operative counselling and post-operative care. None of them were involved in compensation claims for work-related CTS, a factor which has been consistently found to correlate with longer periods off work.
Post-operative care
Individual surgeons have widely varying opinions on post-operative care after carpal tunnel surgery. There is a Cochrane review devoted to the topic which found limited evidence for:
1) Immobilisation - this used to be fashionable but has rather fallen out of favour with most surgeons now. A fairly recent review of the topic (Isaac 2010) concluded that there was no convincing evidence that post-operative immobilisation results in superior outcomes
2) Exercises - this seems directly contradictory to 1) and it is not clear exactly what sort of exercises might be most beneficial. A 'third way' which is now adopted by many surgeons may be termed 'early mobilisation' - patients are encouraged to move the hand and wrist normally as soon as possible after surgery but no specific exercises are recommended
3) Cold therapy/Icing - the conclusion seems to be mainly based on a single study comparing two different methods of cooling the hand after surgery (Hochberg 2001) both of which were combined with narcotic analgesia. Patients treated with an elaborate thermostatically controlled cooling blanket reported less pain at 3 days after surgery than those simply given ice-packs to use intermittently. It is hard to see how this study tells you anything about the usefullness of cooling in improving the outcome of surgery.
4) Electrical Stimulation - this is not really a true post-operative intervention but more something extra done as part of the surgical procedure. The study referred to (Gordon 2010) used a brief period of electrical stimulation of the median nerve immediately after surgery, using electrodes which were inserted next to the nerve during the operation. The nerve was stimulated for one hour after closure of the wound and the stimulating electrodes were then pulled out. The claimed differences in outcome were neurophysiological measures of very limited relevance for the patient.
5) Laser therapy - one placebo controlled randomised study was included (Alves 2011). This seems to have shown no significant difference between the active and placebo groups on any outcome measure
6) Scar desensitisation - As for laser therapy, the summary of the one, unpublished, study which seems to underlie the conclusion in the review abstract (Powell 2003) appears to show no significant differences between the treatment and control groups
7) Arnica - Homoeopathic remedies are well suited to rigorous, randomised controlled trials. There are two good quality studies of this, one controlled trial versus placebo (Jeffrey 2002) and one comparing two different doses and placebo (Stevinson 2003). The first study found slightly less pain in the active group than the control group at 2 weeks (though not at one week). There were no other significant differences. In the second study there were no significant differences in any of the measured outcomes between the three groups. I would have to take issue with the authors of the Cochrane review on this one. I do not think these studies provide 'limited support' for the effectiveness of Arnica. They are some of the better studies included in this review and I would summarise their findings as 'Arnica probably has no effect on the outcome of carpal tunnel surgery'
Many studies however used multiple interventions, often with unsatisfactory control groups, making it very hard to disentangle the effects of single therapies in order to test the effect of any one intervention. A good example of this is (Pomerance 2007) - a study which treated one group of patients simply with a recommendation for some exercises to be done at home and a second group with a therapist directed programme of interventions - 6 sessions of nerve gliding, range of motion and strengthening exercises, massage and 'fluidotherapy'. No difference in outcome was observed in the more intensively treated group.
A pilot study suggested that a programme of 'sensory relearning' - essentially practice at discriminating different textures, shapes and sensations with the fingers (Jerosch-Herold 2012) after surgery might improve sensory recovery but the follow-up definitive study has now been published and failed to demonstrate the same benefit (Jerosch-Herold 2016)
In the absence of any very clear evidence to favour one post-operative regime over another our current recommendations for what to do after surgery can be read in the 'information for Kent Patients' section, but every patient should follow their own surgeon's recommendations on post-operative care. We favour early mobilisation with only a short period in a bulky dressing. Exercises probably do no harm and may be recommended for home use but do not need to be supervised by a physiotherapist. Firm massage of the scar during the healing period MAY help to reduce scar tenderness and thickening but needs to be studied systematically.
Long-term outcome of surgery. Patients often ask -"If I have it operated will it fix the problem for good?". This question is probably commoner nowadays because a quick search of the internet for carpal tunnel syndrome yields many patients complaining about persistent or recurrent symptoms. The issue of persistent symptoms after surgery is covered at length in the failed surgery page but late recurrence of the CTS after initially successful surgery is a different topic about which very little is known. Everyone who sees lots of CTS cases will come across the occasional patient who had surgery 10-20 years previously and who now turns up in the clinic with the same problem again. It is possible that this very small group of patients may only represent the most severe end of a spectrum of recurrent symptoms.A few papers have now appeared in the scientific literature specifically looking at long-term recurrences, with quite widely varying findings:
(Nancollas 1995) reviewed 60 cases an average of 5.5 years after surgery 57% of individuals noted some return of pre-operative symptoms, beginning at least 2 years after surgery, though in almost all of these patients the recurrent symptoms were not severe enough for them to seek medical attention.
(Katz 1995) reported 8 of 35 patients (22%) to be worse at 27 months follow up than before surgery
(Papachristos 2006) provided an update on a long running series of endoscopic decompressions. There are several previous reports of this series but by 2006 it involved 3206 operations on 2247 patients. This series of operations seems to have a long-term rate of 'unsatisfactory outcomes' at 5 years or more of 6.1%
(Hankins 2007) reported a 3.7% recurrence rate by 10 years after original surgery in 2163 patients
(Atroshi 2009) followed up 128 patients for 5 years and reported 21 (16%) with persistent pain and 6 (4.7%) requiring repeat surgery
(Louie 2013) followed 113 patients for an average of 13 years - 13% had significant residual symptoms (expressed as an SSS score of >2)
Tang (2017) reported 9 year follow-up of 40 patients/80 operations (all bilateral cases). 72.5% were completely asymptomatic, suggesting that a quarter of these patients had some form of symptoms long after surgery.
Not all of these studies are concerned with true recurrence of CTS. Some of them are reporting the incidence of long term problems after surgery which may in fact be side efects of the operation rather than recurrence of CTS. The best indicator of recurrent CTS is probably re-operation which is only likely to be undertaken if the surgeon thinks that the nerve is becoming compressed again. I would therefore take the estimate from Atroshi 2009 of a roughly 1:20 (5%) risk of recurrence by 5 years as the best available figure for now - though none of these studies are entirely satisfactory in addressing this question.
Revision date - 21st February 2022
